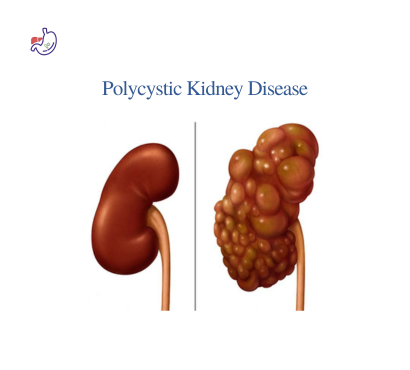
What is Polycystic Kidney Disease? The Silent Cyst Multiplier
Polycystic Kidney Disease (PKD) represents the most common inherited kidney disorder, where hundreds of fluid-filled cysts progressively replace normal kidney tissue. These cysts enlarge kidneys 2-4x normal size, distort architecture, and impair filtration over decades.
Two forms:
- ADPKD (90% cases): Adult onset, dominant inheritance
- ARPKD: Rare childhood form, recessive
India prevalence: ~1:1000 (underdiagnosed); family clusters common.
Genetic Roots: Why Your Family History Matters
ADPKD: PKD1 (85%, severe) / PKD2 (15%, milder) gene mutations → defective cyst regulation proteins.
Inheritance: 50% risk each child if one parent affected
Penetrance: 100% by age 80 (cysts visible ultrasound)
ARPKD: PKHD1 gene; both parents carriers (25% risk)
Severity: Newborn respiratory distress → childhood ESRD
De novo mutations: 5-10% no family history.
Early Warning Symptoms: What Families Notice First
Silent progression 20-40 years → symptoms:
- High blood pressure (60-70% first sign, age 20-30)
- Flank pain (cyst rupture/bleeding/stones)
- Hematuria (gross blood urine episodes)
- Palpable kidneys (abdominal mass)
- Recurrent UTIs (cyst infections)
Advanced: Fatigue, edema, anemia (ESRD approaching).
The Classic Pain Episode: Cyst Rupture Crisis
Sudden sharp flank pain + hematuria = cyst hemorrhage (30% lifetime).
Triggers: Minor trauma, contact sports, jarring
Duration: 1-7 days self-limited
Red flags: Persistent >2 weeks, fever, dropping Hb = CT urgent
Prevention: Contact sports avoidance, seatbelts always.
High Blood Pressure: PKD’s Silent Partner
Mechanism: Cyst compression → renin release → hypertension.
Timeline: Precedes GFR decline by 10-20 years
Target: BP <130/80 slows progression 30% (REIN study)
Drugs: ACEi/ARB first line (renoprotective)
India challenge: Salt-heavy diet accelerates.
Diagnostic Roadmap: From Suspicion to Confirmation
Family history + symptoms → Ultrasound screening (age 18-30):
ADPKD criteria:
Age 15-29: ≥3 cysts (uni/bilateral)
Age 30-59: ≥2 cysts each kidney
Age ≥60: ≥4 cysts each kidney
Advanced:
- CT/MRI: Cyst burden, complications
- Genetic testing: PKD1/PKD2 (₹25-40k)
- GFR/creatinine: Function staging
Disease Progression: The 4-Stage Timeline
| Stage | GFR | Symptoms | Management |
| 1-2 | >60 | HTN, pain | BP control, screening |
| 3 | 30-59 | Proteinuria, anemia | Tolvaptan?, ACEi |
| 4 | 15-29 | Edema, fatigue | Prep dialysis/transplant |
| 5 | <15 | Uremia | RRT (dialysis/transplant) |
ESRD: 50% ADPKD1 by age 58; 70% by 80.
Disease-Modifying Treatments: Slowing the Cyst Tsunami
Tolvaptan (V2 receptor antagonist):
- REDUCE trial: Slows GFR decline 26% first 3 years
- India: ~₹50k/month (insurance coverage varies)
- Side effects: Liver monitoring, polyuria
Somatostatin analogs (lanreotide): Cyst growth inhibition (CREST trial).
Blood Pressure: The Single Biggest Lever
HALT-PKD: Intensive BP <120 systolic → albuminuria ↓58%, LVH ↓30%
ACEi/ARB combo: Mandatory unless hyperkalemia
Salt: <5g/day (Indian challenge: pickles, restaurant food)
Pain Management: Beyond Pills
Chronic ache (cyst pressure): Tramadol, gabapentin
Acute rupture: NSAIDs (caution CKD), ER if severe
Lifestyle: Yoga, weight control, avoid contact sports
Cyst aspiration/decompression: Refractory cases only.
Complications: The PKD Cascade
Kidney:
- Stones (20%, uric acid)
- Infections (pyelonephritis)
- Gross hematuria
Extrarenal (40% ADPKD):
- Liver cysts: 80% age >30 (women > men)
- Intracranial aneurysms: 8-12% (screen if family stroke/SAH)
- Heart valves: Mitral prolapse
- Diverticula: Colon
Pregnancy: HTN worsens; screen preconception.
Lifestyle: Your PKD Progression Brake
Diet:
Low salt <5g
Normal protein 0.8g/kg
Alkalinize urine (citrate)
Avoid high oxalate (spinach)
Exercise: Aerobic 150min/week (no contact)
Weight: BMI <25 (obesity accelerates)
Smoking: Absolute NO (vascular damage)
Hydration: 3-4L/day (vasopressin suppression)
Family Screening: Break the Inheritance Chain
Protocol:
Age 18-30 at risk: Annual BP + ultrasound
Age <18: Only symptomatic/genetic counseling
Spouse: Routine (dominant inheritance)
Genetic counseling: IVF-PGD for known carriers.
End-Stage Management: Planning Ahead
Dialysis: Start GFR <10-15 (symptoms guide)
Transplant: Excellent outcomes; living donor preference
India stats: 1L dialysis patients; transplant wait 3-5 years
Advance care: Discuss early (age 40+).
Children & ARPKD: Different Ballgame
Newborn: Enlarged kidneys → respiratory distress
Childhood: Growth failure, hypertension
Prognosis: 30% ESRD by age 10
Prenatal: Oligohydramnios → lung hypoplasia.
India-Specific Challenges
Diagnosis delay: Incidental ultrasound finding common
Genetic testing: Limited centers (Mumbai, Delhi)
Tolvaptan: Cost prohibitive (<5% access)
Transplant: Living donor shortage
Hypertension: Poor screening rural areas
Patient Timeline: From Diagnosis to Management
Year 0: Diagnosis (ultrasound, genetic)
Year 1-5: BP control, annual USG/GFR
Year 5-15: Tolvaptan candidate?, pain mgmt
Year 15-25: Transplant planning
Hopeful Outlook: Research Pipeline
Ongoing trials:
- Metformin (mTOR inhibition)
- Anti-inflammatory (tofacitinib)
- Vasopressin antagonists (lixivaptan)
Prognosis improved: Strict BP → ESRD delayed 10-15 years.
FAQ
- Can lifestyle changes stop PKD progression?
Slow 20-30%: BP <120/80, BMI <25, no smoking, 3L water. Tolvaptan adds 26% in the first 3 years. Combined approach best. - Should family members get tested for PKD?
Yes age 18+: Annual BP + ultrasound if parent is affected. Early HTN detection prevents 50% damage. Children only if symptomatic. - Is kidney transplant a cure for PKD?
Not cured – cysts remain native kidneys. Transplanted kidney functions normally 15-20 years. Recurrence native disease kidneys no